Whether or not you’re for or against weight loss medications, I can assure you they’re here to stay. I estimate that 35-40% of my patients are currently taking these medications, and that estimate only includes those who openly disclose their use.
Despite their tremendous impact on Obesity, Diabetes, and Sleep Apnea it comes with a severe financial challenge. The current math simply isn’t sustainable with cost estimated to be $71.7 billion in 2023.
Set It and Forget It: The Most Expensive Mistake in GLP-1 Care
In my clinic, I frequently encounter patients who began GLP 1 therapy months ago but are frustrated because they have lost little or no weight. My first question is
“Have you increased the dose?
The answer is depressing because most arnswer
No. I am still at the starting dose, long after initiation despite not having side effects.
Healthcare is Acting Like a Dumb Thermostat
For those who remember the old “dumb thermostats”, there was usually one person in the house, maybe your dad or mom, who was allowed to touch it. Everyone else knew it was off-limits. If you were cold or hot, you had to wait until the “thermostat authority” decided it was time to adjust.
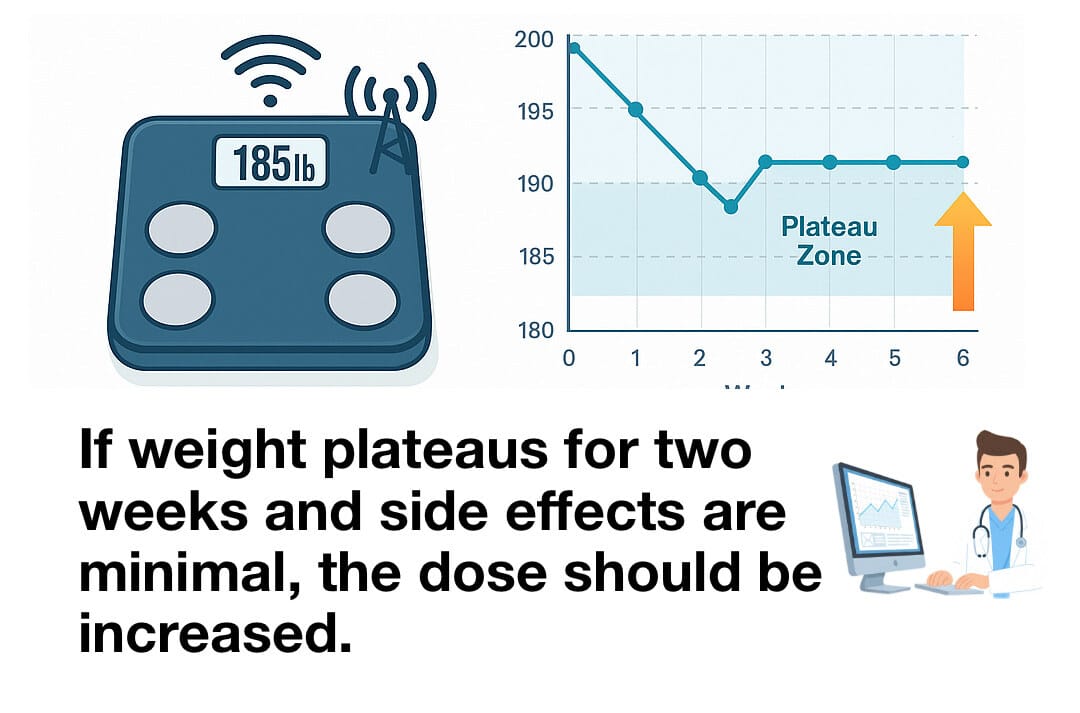
Medication management often works the same way. The dose just stays the same until the “medical authority” makes an adjustment. Unfortunately, dose adjustments for blood pressure, diabetes, or weight loss happen only during scheduled, face-to-face visits. Until that appointment, patients stay stuck at the same dose, even when the data says it’s time to change.
A Smarter Way: Wearable Supported GLP 1 Care that is Continuous
What if we built a model to guide therapy that is continuous and adaptive? Smart scales, wearables, and intelligent protocols can turn every patient into a real-time feedback loop and every dose into a decision guided by evidence, not a calendar.
Building a Smart Thermostat for GLP-1 Care
Our homes already know how to self-correct, and when programmed well, they save us money.
GLP-1 therapy should work the same way and save the Healthcare System Money
When weight plateaus the system should respond immediately with increased dose.
Side Effects reported using App based messaging -> Hold dose; reinforce mitigation (meal pacing, hydration, antiemetics, fiber, PPIs if needed).
If weight loss >5% in 1 month OR sarcopenia risk → hold titration; evaluate nutrition and exercise plan.
Monthly telehealth coaching visits with Avatar based dietitian for diet, exercise, and behavioral support with wearables constantly tracking the amount of resistance training performed.
Administer Mental Health Questionnaire for early signs of depressive symptoms or changes in mood that may impact adherence, engagement, or overall well-being
For payers, health systems, and digital health leaders, this is the path from high cost to high value. Our Homes are Smart but are Healthcare at Home is Dumb. Its time for a Renovation and Revolution in Healthcare.
If our homes can adjust in real time, our healthcare should too. We can keep setting it and forgetting it, or we can finally learn from the thermostat.
#Wearables #GLP1 #DigitalHealth #ObesityCare #MetabolicHealth #RPM #Semaglutide #Tirzepatide #ValueBasedCare #HealthEconomic Eli Lilly and Company Novo Nordisk
